
What is a retinal detachment?
When you develop a retinal detachment, your retina (or more specifically, your neurosensory retina) becomes peeled off from the wall of the eye.
This is similar to when the wallpaper peels away from your living room wall. If your detached retina is not repaired, you will eventually lose all your visual function in that eye.
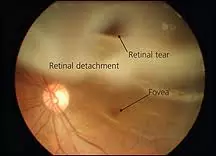
The only way to fix a retinal detachment (example on the left) is to undergo retinal detachment surgery. The success rates are higher the earlier surgical repair is performed. The later you postpone surgery, the greater the chances of surgical failure due to scarring from proliferative vitreoretinopathy.
Most of the time, you will have a good outcome if any retinal detachment surgery complications are dealt with promptly and managed properly. Some complications are more difficult to manage than others, and may require repeat surgery and/or frequent outpatient visits.
It is important that you listen and adhere to the advice given to you by your ophthalmologist regarding your eye drops and general care after surgery. Doing so reduces the risk of complications and increases the chance of success of your operation.
In general, retinal detachment surgery complications can be classified into early (within 2 weeks of surgery) and late (after 2 weeks postoperatively) complications.
Early retinal detachment surgery complications
Increased pressure in the eye (raised intraocular pressure): This can be uncomfortable, and happens in around 10% of the time. If the pressure increase is high, you may experience blurring and aching around the eye, as well as nausea and sickness. The raised pressure is usually temporary.
Depending on how high the eye pressure is, your ophthalmologist may give you eye drops or tablets to bring the pressure down. This usually does not cause any lasting damage unless the eye pressure is elevated to a very high level or if you already suffer from glaucoma.

Measurement of the intraocular pressure is important during the postoperative period after surgery. If you had gas inserted into the vitreous cavity of your eyeball, you must not to go on any flights for the next few weeks after surgery. Flying causes the gas in your eye to expand and increase the eye pressure tremendously. This is very painful and bad for your optic nerve.
Infection of the eyeball (endophthalmitis): Endophthalmitis is one of the most dreaded complications of any ocular surgery surgery. It is extremely serious, and you can lose your vision permanently.
How would you know if you have endophthalmitis? Well, your eye will be extremely painful and you will have very poor sight. There may be yellow discharge from the eye and you may even see a yellow fluid level in the eyeball (hypopyon).
This condition is an ophthalmic EMERGENCY, so please do not wait and see “if it gets better over the next few days”. It won’t. Your eye needs immediate injection of antibiotics into the eyeball.
You will most likely be admitted to hospital for intensive eyedrops and oral medications. The earlier treatment is started, the better the chances of retaining good vision. However, it can take several months before the eye settles down.
Postoperative infective endophthalmitis is one of the worst possible retinal detachment surgery complications that can occur. This is infection affecting the entire eye, and if not treated expediently with antibiotic injections into the vitreous cavity, will result in permanent blindness. Note the yellow fluid level or hypopyon in this eye.

Luckily, this condition is very rare (less in 0.1%) due to the meticulous cleaning and infection control techniques.
If you have a condition that lowers your immune system and predisposes towards infection, highlight it to your ophthalmologist so that even more precautions can be taken to prevent infection.
Late retinal detachment surgery complications
Retinal re-detachment: Despite what seemed like initial successful surgery, the retina can become detached again. This will necessitate repeat surgery to try to correct the retinal detachment. Retinal re-detachments can occur due to a variety of reasons, including:
– Re-opening of old retinal breaks
– Formation of new retinal breaks
– Proliferative vitreoretinopathy
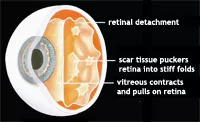
Proliferative vitreoretinopathy (PVR) (see left) causes scarring of the retina. Normally a thin and pliable lining, the retina becomes thickened, wrinkled and difficult to remain attached to the wall of the eye. PVR occurs in up to 10% of retinal detachments, and is a major cause of retinal re-detachments.
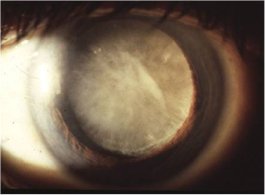
Cataract: A cataract (see right) develops when the natural lens becomes cloudy, and this occurs naturally with age. Surgery itself, insertion of gas or oil in the vitreous cavity, and the use of steroid eye drops encourages cataract formation. Cataract surgery may be needed as soon as a few months after surgery.
Buckle-related complications: Sometimes, a scleral buckle is required to repair a retinal detachment. This technique uses a piece of plastic or silicone or sponge as a buckle to press on the outside of the eye. This creates external pressure which causes the sclera to ‘buckle’ inwards and forces the wall of the eye to press against the detached retina.
Because the buckle is placed around the outside of the eyeball, it can sometimes interfere with the way your eye muscles work. The buckle may limit the movement of the muscles that control eye movement.
If this happens, you will experience double vision (also known as diplopia). Most of the time, your eye muscles eventually adapt and the double vision becomes less of a problem over time. The buckle can also erode the surrounding eye tissues, causing irritation and recurrent infections.


