
Why is pterygium surgery necessary?
Pterygium excision is performed for patients who have developed a pterygium that is causing irritation or visual impairment. Conjunctival autograft is performed to reduce the risk of recurrence of the pterygium.

A pterygium (plural: pterygia) is a benign growth of the conjunctiva (skin of the eye) that grows towards the cornea (front window of the eye). In some more aggressive cases, the pterygium grows onto the visual axis of the cornea, causing visual impairment.
Sunlight damage is one of the most important risk factors a pterygium to develop and progress.
Surgical excision and conjunctival autograft is currently considered the gold standard procedure to treat a pterygium. The recurrence rate following surgery is low, ranging from 5% to 10%.
What does pterygium surgery involve?
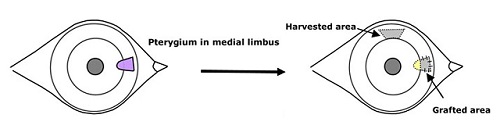
Pterygium excision and conjunctival autograft is a surgical procedure which involves:
● Using a scissors to cut the pterygium from the adjacent conjunctiva
● Using a scissors or blade to excise the pterygium from the corneal surface
● Harvesting a piece of healthy conjunctiva from the top of the eye
● Transplanting the healthy conjunctiva to cover the defect that has been
created in the process of removing the pterygium
● Using dissolvable stitches to hold the conjunctival graft in place.
What are the potential risks?
This procedure is generally safe. Most complications can be treated although sight-threatening complications may occur rarely (less than 1 in every 1000). Risks include:
● Bleeding around the eye. This usually settles gradually over a few weeks.
● Discomfort due to stitches. The stitches will take up to 6 weeks to dissolve.
● Scarring and astigmatism of the cornea affecting vision.
● Recurrence may occur despite the conjunctival autograft.
● Infection inside the eye (endophthalmitis). This is the most serious
complication and may cause permanent sight loss.
What should I expect?
Pterygium excision and conjunctival autograft is a hospital-based day case procedure performed under local anesthetic. The operation is usually performed one eye at a time.
Before surgery:
On the day of your procedure, please take all your usual medications unless otherwise advised. You will need to fast for at least 6 hours before your procedure. You will not be able to drive home on the day of the procedure, so you will need to arrange for someone to take you home. Please allow at least 3 to 4 hours in the hospital.
During surgery:
To reduce the risk of infection, povidone iodine antiseptic is used to clean your eye and eyelashes, a sterile drape will cover your face, and a sterile clip will keep your eyelids open.
You will be awake during surgery, but you should not feel any pain. You may notice bright lights or colours, hear buzzing sounds, and feel cold water running down your cheek or ear.
You will need to lie relatively still for up to 45 minutes for the operation. At the end of surgery, you may feel a sting due to an injection.
After surgery:
After surgery, a pad and shield will be placed over your eye. The pad and shield can be removed the next day, and you can start your postoperative eye drops, usually a steroid (Prednisolone or Dexamethasone) and an antibiotic (Chloramphenicol) 4 times daily for 3 to 4 weeks. Please continue your other usual eye drops.
Over the next few days, you may experience blurriness, discomfort, sensitivity to light, and blood around the eye. These will gradually improve over the next few weeks with the eye drops. You may take paracetamol to help control any discomfort.
You will usually be reviewed 1 to 2 weeks after surgery. There is no need to be seen the next day unless there is a specific clinical reason to do so.
Please contact the clinic immediately if you experience pain or a sharp drop in vision.


