What is glaucoma and why is it important?
nerve, usually related to high pressure in the eye. This causes visual field loss and if untreated, eventual blindness.
Glaucoma is the second commonest cause of blindness worldwide, and affects at least 2% of the population. It is a major eye health issue, and the most worrying thing is that most sufferers do not know that they have this condition.This is because you usually do not notice any glaucoma symptoms until a lot of glaucoma damage has already occurred.
Unfortunately, glaucoma cannot be ‘cured’ or ‘reversed’, despite the many claims to the contrary that are widespread throughout the internet. Any vision lost from the optic nerve damage cannot be recovered.
The only proven glaucoma treatment option available currently is to reduce the eye pressure, and this can be achieved through eye drops, laser, or surgery.
Please remember that reducing the eye pressure does not restore your vision; it only serves to slow down and reduce the risk of further eyesight deterioration. Hence the focus on monitoring: early detection means early glaucoma treatment and less glaucoma blindness.
See Related: Glaucoma treatment with eye drops and medications
The aim of glaucoma treatment is to reduce the eye pressure in order to prevent further worsening of the visual field. The tunnel vision effect from advanced peripheral field loss is well demonstrated in the example above.
I’ve been diagnosed with glaucoma. I’ve been told I need glaucoma surgery but idont understand why.
Most patients with glaucoma are treated with eye drops or laser, or a combination of both. These glaucoma treatments reduce the eye pressure to protect the optic nerve from further damage. The idea is to slow down and reduce the risk of further eyesight deterioration.
However in some patients, these glaucoma treatments are not able to reduce the eye pressure enough. The pressure remains stubbornly high and the glaucoma continues to cause damage to the optic nerve.
This is where glaucoma surgery comes in. Surgery is generally reserved for those in whom eye drops and laser treatments are unable to reduce the eye pressure sufficiently to an acceptable level. In other words, glaucoma surgery is needed to reduce the eye pressure when the other glaucoma treatment options have failed.
Glaucoma filtering surgery is usually only required in 5% of those with glaucoma. The types of glaucoma that are more likely to need surgery include pseudoexfoliation glaucoma, uveitic glaucoma, neovascular glaucoma, and traumatic glaucoma.
What are the options available for glaucoma filtering surgery?
There are 3 main types of glaucoma filtering surgery: trabeculectomy, non-penetrating glaucoma surgery, and glaucoma tube shunt implantation.
These operations can be performed with a local anesthetic injection or with general anesthetic where you are put to sleep. Surgery can take up to 90 minutes to complete.
Continued use of intraocular pressure lowering eye drops is normally not needed following surgery in 50% of cases. You may need to use steroid eye drops for an extended period of time to reduce the amount of inflammation and scarring in the eye after surgery.
Which type of surgery most suits you would depend on a few factors, such as the type of glaucoma that you have, the risk factors for failure, and whether there is an increased risk of complications. Your ophthalmologist will discuss with you the surgery method that will best be able to reduce your eye pressure and keep the pressure stable.
1. Trabeculectomy – the gold standard glaucoma surgery
Trabeculectomy is the most common type of filtration surgery to reduce eye pressure. It also happens to be the gold standard operation for glaucoma. Trabeculectomy has been around since the 1950s, although there have been many modifications to the original surgical technique.
With a trabeculectomy, a new channel is created in the wall of the eye. This allows fluid to drain from inside the eye to the outside, forming a pocket on the surface of the eye (this is called a bleb). It can be performed for almost all types of glaucoma.
Modern trabeculectomy is safe and effective, with a success rate of around 80 to 90%. It is the first line surgical treatment for glaucoma. A patient with a successful trabeculectomy procedure can expect pressures between 8 mmHg to 16 mmHg without any eye drops.
Now, who wouldn’t want pressures between 8-16 mmHg without eye drops? So why isn’t every glaucoma patient rushing to have trabeculectomy?
The first reason is the potential risk of complications. I do not recommend trabeculectomy surgery lightly. Most risks are minor and can be managed with eye drops or laser or revision surgery. However, there are more serious risks that can cause visual impairment, and more rarely, blindness. Patients who have had trabeculectomy will need lifelong monitoring for the risk of infection from the bleb.
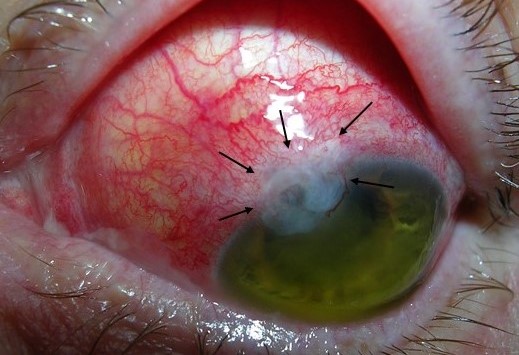
The picture above shows an inflamed bleb (black arrows). This needs to be examined urgently by an eye specialist to exclude potentially sight-threatening infection.
The second reason is the intensive management and follow-up after surgery. The main cause of failure of trabeculectomy is scarring over the surgery site. This is why you will need to use anti-inflammatory eye drops every 1-2 hours during the initial few weeks.
Depending on the examination findings during your post-operative visits, you may also need to have additional injections of anti-scarring medication over the surgical site. In general, you will need to attend for review at least once every 1 to 2 weeks for the first couple of months after trabeculectomy.
In general, the recovery period after trabeculectomy is around 2 to 3 months.
See Related: Patient’s guide to glaucoma treatment with trabeculectomy
2. Non-penetrating glaucoma surgery
Non-penetrating glaucoma surgery is much less commonly performed compared to glaucoma. It is suitable only for open angle glaucoma. If you have angle closure glaucoma, then this procedure will not work for you. You’ll need to undergo trabeculectomy or glaucoma tube shunt implantation instead.
This procedure is very similar to trabeculectomy in technique. The main difference is that there is no actual channel or hole is created in the wall of the eye (hence the term ‘non-penetrating’). Instead, only a thin membrane (called the roof of Schlemm’s canal) is removed. This still allows aqueous to exit the eye, but in a more controlled manner.
The 2 main non-penetrating glaucoma surgery techniques are deep sclerectomy and viscocanalostomy.
In general, the recovery period after non-penetrating glaucoma surgery is around 2 to 3 months.
Which is better? Non-penetrating glaucoma surgery or trabeculectomy?
And the answer is: it depends.
The 2 main potential benefits of non-penetrating glaucoma surgery over trabeculectomy are: less risk of infection and less risk of hypotony (where the pressure becomes too low). This may be beneficial if you are prone to infections or at risk of low eye pressure after surgery.
The 2 main drawbacks are: you may not be able to achieve a low enough pressure compared to trabeculectomy, and you still have to undergo the same intensive management and follow-up as for trabeculectomy.
3. Glaucoma tube shunt implants
Drainage implants or glaucoma tube shunts are tubes that are implanted into the anterior chamber of the eye, which allow aqueous to drain out of the eye.
Traditionally, glaucoma tube shunts are implanted if a trabeculectomy operation has failed. However, they are now increasingly implanted as first line glaucoma surgery in certain circumstances. These include if you are at high risk of conjunctival scarring or if you are unable to undergo the intensive postoperative management that a trabeculectomy demands.
There are 5 main glaucoma tube shunts: the Ahmed valve, the Baerveldt tube, the Krupin valve, the Molteno tube, and the Paul tube.
In general, the recovery period after glaucoma tube shunt implantation is around 2 to 4 months.
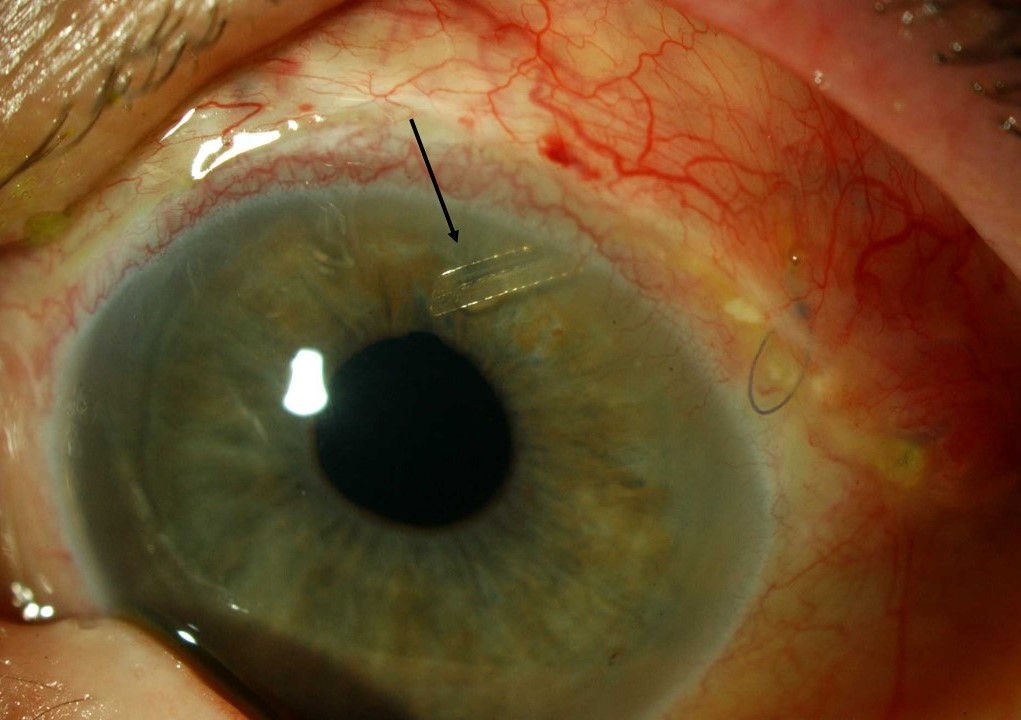
The picture above shows a well-positioned glaucoma tube shunt in the anterior chamber of the eye (black arrow).
Which is better? Glaucoma tube shunt implantation or trabeculectomy?
And the answer is, yes, you guessed it: it depends.
The main benefit of the glaucoma tube shunt over trabeculectomy is that the postoperative management is not as intensive and is less susceptible to failure from scarring. This operation may therefore be suited to you if you live a long distance from care, or if you scar easily (hence trabeculectomy is very likely to fail if performed in your eye).
However, the pressure is unlikely to be as low as a trabeculectomy, and you have extra risks that trabeculectomy does not have. These extra risks include double vision due to eye movement problems, damage to the cornea due to contact from the tube, and pain due to erosion of the tube.
See Related: Patient’s guide to glaucoma treatment with tube shunts
My friend had glaucoma treatment with MIGS and apparently it was very successful. What is MIGS?
More recently, a new class of glaucoma surgery called minimally invasive glaucoma surgery (MIGS) is becoming increasingly popular.
MIGS can be performed as an independent procedure, but is normally performed in conjunction with cataract surgery. It is ideal if you want to reduce the number of eye drops you use, or if you need your pressure lowered but are wary of the risks of traditional glaucoma filtering surgery.
Multiple MIGS procedures have now been introduced in Australia and worldwide. These include the iStent, Hydrus micro-stent, XEN gel stent, PreserFlo microshunt implant, ab-interno canaloplasty, endocyclodiode photocoagulation, with still more on the way.
Most work by enhancing drainage of aqueous out from the eye, apart from endocyclodiode photocoagulation, which works by reducing production of aqueous from the ciliary body.
The main advantages of MIGS the traditional glaucoma filtering surgery are that MIGS is less invasive, is quicker to perform, has a faster recovery period (of 4 to 6 weeks), and has less risk of complications.
As an example, a trabeculectomy will take approximately 45 minutes to complete. An iStent implantation procedure, as you can see in the video below, will take less than 5 minutes. Implanting the Hydrus micro-stent and XEN gel stent will take around 10 to 15 minutes.
See Related: Patient’s guide to glaucoma treatment with the iStent
Shouldn’t I have MIGS then? It sure sounds better than having a trabeculectomy!
Again, it depends.
Yes, there are many advocates for MIGS due to its many advantages, but trabeculectomy is the gold standard glaucoma surgery for a reason. And that reason is its unparalleled ability to reduce the eye pressure safely and consistently.
At the moment, none of the MIGS procedures are able to reduce the eye pressure as much as trabeculectomy, save perhaps the XEN gel stent or PreserFlo microshunt in certain circumstances.
The current guidelines therefore recommend MIGS as a suitable treatment for mild to moderate glaucoma, while glaucoma filtering surgery is more appropriate for advanced glaucoma.
Patient’s guide to glaucoma treatment with the Hydrus
Patient’s guide to glaucoma treatment with the XEN stent
And finally, three tips to help with your postoperative recovery after glaucoma surgery
Although effective at lowering eye pressure, glaucoma surgery is also effective at causing complications. If you are at all concerned about how your eye is feeling after surgery, please contact your ophthalmologist for a review.
Tip #1: Follow your postoperative instructions, particularly when it comes to eye drops. If your surgeon says instil your steroid eye drops every 2 hours, please instil your steroid eye drops every 2 hours. The instructions are there for a reason. They are not there to deliberately inconvenience you. If you are unable to instil the eye drops, or have concerns about potential side effects, please contact your ophthalmologist for a solution or alternative.
Tip #2: Please resist the temptation to rub your eye. Yes, your eye will be blurry, uncomfortable, itchy or feel as if there is something in the eye. It is normal to feel all this after surgery. As your eye settles and the stitches dissolve, your eye will feel better. Rubbing the eye may potentially increase your risk of complications, including infection and hypotony. You can continue wearing your eye shield at night if you are worried that you may accidentally rub your eye while you are asleep.
Tip #3: Make sure you are not deficient in vitamin D. There is increasing evidence that low vitamin D levels increase the risk and severity of scar development. Remember what we discussed about scarring and risk of glaucoma surgery failure? Taking vitamin D supplements is therefore an easy way to help reduce the risk of scarring and ensure success of your glaucoma surgery.
See Related: The six best glaucoma supplements for your optic nerve