
What is temporal arteritis or giant cell arteritis?
Temporal arteritis, also known as giant cell arteritis, is an inflammatory condition that affects the medium to large arteries in the body. It is a systemic condition, which means that any medium to large artery in any part of the body can be affected. This includes the eye, brain and heart.
The most frequently affected artery is the superficial temporal artery, hence the name. When the temporal artery is inflamed, it becomes more prominent, knobbly and tender to touch.
This condition is also called giant cell arteritis because the inflammation is characterized by the presence of giant cells when analyzed with a microscope. To this day, nobody really knows why this inflammation occurs.
Temporal arteritis occurs in around 1 in 5000 adults over 50. It seems to be most common after the age of 75. Women are more prone, being 2 to 3 times more likely to suffer from giant cell arteritis than men.
How does it cause blindness?
The underlying disease process is inflammation of the arteries. Inflammation causes the arteries to become clogged up, so that oxygen and blood can no longer be delivered to the tissues that the arteries supply. Ultimately, this will result in tissue death.
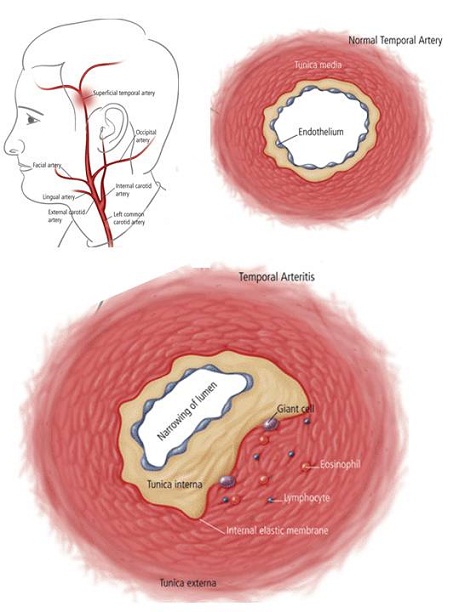
Diagram demonstrating how inflammation from giant cell arteritis causes arteries to become blocked to the extent that blood flow becomes interrupted.
Top left: Location of the superficial temporal artery.
Top right: A normal healthy artery with a wide opening (lumen) that allows fresh blood to pass through easily and without much restriction.
Bottom: An inflamed artery, with a significantly narrowed lumen that limits the flow of blood.
If you have temporal arteritis which is untreated, you have a 60% to 70% risk of having your vision affected in one eye. Having an affected eye increases the risk of the other eye becoming involved to 100% if left untreated. In other words, you run the very high risk of becoming blind in both eyes if not treated as a matter of urgency.
The 2 main blinding complications are: arteritic ischemic optic neuropathy and central retinal artery occlusion.
Arteritic ischemic optic neuropathy: This occurs when the artery that provides blood to the optic nerve becomes so inflamed that it is no longer able to deliver sufficient amounts of fresh blood to the nerve. The optic nerve is starved of blood and becomes damaged from ischemia. Unfortunately, this damage and its effect on the vision is not reversible once it happens.
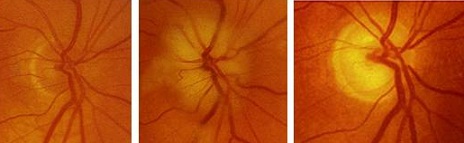
Left: The appearance of a healthy, pink optic nerve.
Centre: The optic nerve becomes swollen due to ischemia (ischemic optic neuropathy).
Left: The optic nerve eventually ‘dies’ and becomes pale (optic atrophy).
Central retinal artery occlusion: This occurs when the artery that provides blood to the retina becomes so inflamed that it is no longer able to deliver sufficient amounts of fresh blood to the retina. The retina is starved of blood and becomes damaged from ischemia. As with arteritic ischemic optic neuropathy, this damage to the retina and its effect on the vision remains permanent.
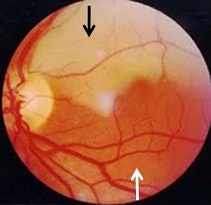
Retinal artery occlusion affecting the top half of the retina. In this example, the artery to the top half of the retina is no longer able to provide fresh blood due to inflammation. The retina is starved of oxygen and becomes swollen. The swelling (edema) of the retina is seen clinically as a whitish pale area (black arrow). The bottom half of the retina remains normal (white arrow).
While giant cell arteritis commonly affects the vision, please do not forget that it can affect any medium-sized or large-sized artery anywhere in your body. So if your coronary arteries become inflamed, you are at risk of developing a heart attack (myocardial infarction). If your cerebral arteries become inflamed, you are at risk of developing a stroke (cerebrovascular event).
So not only is temporal arteritis a sight-threatening disorder, it is also potentially a life-threatening disorder.
How is temporal arteritis diagnosed?
In 1990, the American College of Rheumatology set out the following criteria for the diagnosis of temporal arteritis:
– Age over 50 years
– New headache over the temple
– Abnormality of the temporal arteries
– Erythrocyte Sedimentation Rate (ESR) > 50 mm/hour
– Positive temporal artery biopsy for the presence of giant cells
If you have 3 of the above criteria, then you most likely have giant cell arteritis and should be started on treatment.
Headache over the temple is a typical symptom of giant cell arteritis. The headache is not one that is felt all over the head. Instead, the pain should be specific and localized to the superficial temporal artery.

Apart from pain in the temple area, you should also be aware of these other tell-tale symptoms of temporal arteritis.
– Pain in your jaw when chewing food (jaw claudication)
– Pain in your scalp when combing hair (scalp tenderness)
– Aching of your shoulder girdle (due to polymyalgia rheumatica)
– Double vision (due to cranial nerve palsy)
If you experience any of the following symptoms, please contact your family doctor or ophthalmologist for further investigations. There are 2 main investigations that are most useful for diagnosing temporal arteritis: blood tests and temporal artery biopsy.
Blood tests: The 2 main inflammatory markers are the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Elevated levels of both indicate the presence of significant inflammation in the body. Your doctor will need to exclude infection, which can also raise the ESR and CRP levels. A normal white cell count suggests the absence of active infection.
Temporal artery biopsy: This is performed under local anesthesia and can take up to 40 minutes. It involves shaving hair from your temple and then making a 1 to 2 inch incision. A small piece of your superficial temporal artery is removed and sent to the laboratory for histopathological analysis. The sutures closing up the wound (see right) can usually be removed after 5 to 7 days.
How is temporal arteritis treated?
The main treatment for temporal arteritis is with corticosteroid tablets, usually Prednisone (Prednisolone). The steroids will reduce the inflammation of the arteries, thereby decreasing the swelling and clogging up inside the arteries. This allows free unimpeded flow of fresh blood to the target tissues. With the optic nerve and/or retina no longer being starved of blood, loss of vision from the inflammation is prevented.
The steroids are usually started at a very high initial dose to hit the inflammation hard and fast. You will need to be monitored very closely for response to treatment and also for any side effects or complications from the steroid treatment. The general side effects of steroids include high blood pressure, stomach ulceration, mood disorders, depressed immune function and diabetes mellitus. Steroids can also affect the eye by causing cataract and glaucoma.
The steroid dose will be gradually reduced over several months. Eventually you may be able to stop the steroid altogether, or if not, be maintained on a very low dose. Giant cell arteritis can recur despite successful treatment, sometimes many years later. You should always be vigilant for its symptoms and consult your doctor if you think you are starting to get a recurrence.
Remember that steroid treatment will not reverse any vision loss that has already occurred. It will, however, help to protect your other eye from the ischemic damage that can be caused by temporal arteritis. As always, early diagnosis and treatment is key to prevent any sight loss to begin with.


