What is thyroid eye disease?
Thyroid eye disease is a condition where the eye muscles and fatty tissues behind the eye in the eye socket (orbit) swell due to an autoimmune disease affecting the thyroid gland.
An autoimmune disease occurs when the body’s immune system recognizes a particular tissue or organ in the body as “foreign”, and mounts an immune response against this tissue or organ. In thyroid eye disease, the autoimmune process attacks and causes inflammation and swelling of the eye muscles and tissues in the eye socket. The reason for this is unknown.
Graves’ disease is an autoimmune disease affecting the thyroid gland, whereby abnormal antibodies stimulate the thyroid gland to cause excessive production of the hormone thyroxine. Graves’ disease is the commonest cause of an overactive thyroid (hyperthyroidism). Thyroid eye disease is commonly associated with Graves’ disease, and hence it is also known as Graves’ orbitopathy. .
Graves’ orbitopathy develops in around 1 in 4 patients with Graves’ disease. It generally occurs in middle age, with twice the risk in smokers. The risk is increased eight times for heavy smokers.
What happens if I get thyroid eye disease?

Typical appearance of thyroid eye disease/Graves’ orbitopathy, with the characteristic bulging eyes and staring look. Note the wide exposure of the surface of the eyes due to eyelid retraction, and the redness of the inside corners of the eyes.
Most of the symptoms and signs are due to inflammation, swelling and congestion of the eye muscles and fatty tissue within the eye socket. Both eyes are usually affected, although not always with the same severity.
With mild thyroid eye disease, you may experience symptoms such as:
● Bulging or staring eyes
● Irritation and grittiness in the eyes
● Dry eyes or watery eyes
● Dislike of bright lights
● Swollen or fullness in the eyelids (could be upper or lower lids)
● Redness of the eyes and eyelids
However, more severe disease can cause significant issues such as:
Diplopia or double vision. This occurs because the eye muscles in the orbit that move the eyeball are so swollen that they cannot function properly. If the inflammation of the muscles are not treated appropriately, the muscles become scarred and the double vision becomes permanent.
Corneal exposure. Sometimes, the swelling in the orbit pushes the eyeball so far forward that the eyelids don’t close properly. This exposes the cornea (front window of the eye), making the eye feel even more dry, irritated, and sensitive to light. Excessive exposure and dryness of the cornea increases the risk of infection and scarring.
Optic neuropathy. In very severe cases, the nerve connecting the eyeball to the brain (optic nerve) can be stretched, compressed and damaged. This is serious because permanent optic nerve damage will cause irreversible loss of vision. Initially, it may cause blurring or colours to appear faded.
How is thyroid eye disease diagnosed?
During your consultation, your ophthalmologist will examine the following:
● Visual function, including visual acuity, color vision, and visual fields
● Eye pressure
● Eye muscle movements
● Optic nerve appearance
You may also need to undergo tests such as:
● Blood tests to check the level of thyroxine and thyroid receptor antibodies
● Thyroid scan to test how active the thyroid is
● MRI or CT scan to look at how swollen the muscles in the eye sockets are
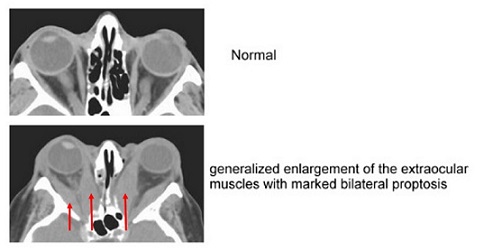
Top: CT scan of normal orbits; Bottom: CT scan of Graves’ orbitopathy. Note the enlarged eye muscles (red arrows) and forward protrusion of the eyeballs (proptosis)
How is thyroid eye disease treated?
This is a complex autoimmune condition that will require management by both an eye specialist (ophthalmologist) and an endocrinologist who specializes thyroid disease.
The main aim of treatment is to reduce the risk of vision loss and double vision by protecting the surface of the eye and reducing the amount of swelling in the eye socket. Treatment options include the following:
Stop smoking. Non-smokers and ex-smokers respond better to treatments than those who continue to smoke. The severity of inflammation and swelling is also less in those who stop smoking.
Maintain thyroid control. Your thyroid levels should be in the normal range and should not have large fluctuations. Make sure you have your regular blood tests and check-ups with your endocrinologist, and follow instructions about when and how to take your thyroid medication.
Lubricant eye drops and artificial tears to alleviate any ocular surface dryness and irritation.
Selenium supplements 100 mcg twice daily for six months has been shown to be beneficial for mild thyroid eye disease.
Prisms can be attached to spectacles to reduce double vision.
High-dose steroid medications, such as prednisolone, are sometimes necessary if there is too much inflammation and swelling in the orbit. These may be taken orally but may sometimes have to be administered via an intravenous drips. The purpose of the steroid medication is to decrease inflammation in the eye muscles and the orbit.
External beam radiotherapy is sometimes considered to reduce the inflammation and swelling in the orbit in active or progressing thyroid eye disease. Typically 20 Gy (2000 Rads), divided over 10 days, is delivered to each orbit. It is safe overall, but risks include hair loss, cataract, retinopathy, and a small lifetime risk of developing tumors.

External beam orbital radiotherapy is not widely available. This treatment can only be delivered in linear accelerator radiotherapy units.
Surgery is sometimes necessary for a variety of reasons. This includes orbital decompression surgery to relieve pressure in the orbit (and prevent compression damage to the optic nerve), eye muscle surgery to realign the muscles and reduce double vision, and eyelid surgery to improve lid appearance.
I have thyroid eye disease. What is my prognosis?
The good news is that the active stage of thyroid eye disease is temporary. Over time, the inflammation and swelling in the orbits will get better, usually over several months to about two years.
The bad news is that the physical changes from thyroid eye disease can be permanent in many sufferers, in particular the bulging eye appearance and the double vision.
Earlier and better control of the inflammation during the active stage means less chance of permanent issues with double vision and vision loss. Therefore you need to seek medical attention without delay if your symptoms worsen, or if you start to notice vision problems such as double vision, blurriness, and faded appearance of colors.