Why is trabeculectomy necessary?
Trabeculectomy is performed for patients with worsening glaucoma or uncontrolled high eye pressure despite being on medications.
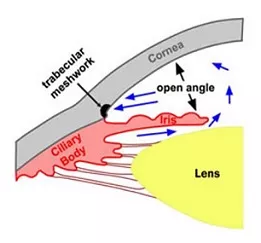
Fluid in the eye (aqueous) is produced by the ciliary body, and drains out through the trabecular meshwork (drainage pathway) in the drainage angle. Sometimes the trabecular meshwork becomes unable to cope, preventing aqueous from draining out easily. This causes pressure to build up in the eyeball. When the pressure in the eye is too high, it can cause optic nerve damage and permanent vision loss – this is called glaucoma.
The trabeculectomy operation reduces eye pressure, which in turn reduces the risk of further optic nerve damage from glaucoma.
Trabeculectomy is currently considered the gold standard surgery to reduce eye pressure.
See Related: Surgical treatments for glaucoma
What does trabeculectomy involve?
Trabeculectomy is a 60 to 90 minute surgical procedure which involves:
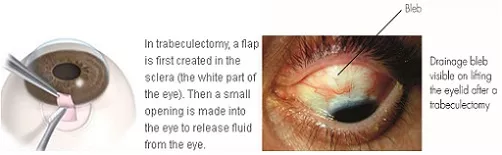
● Making a trap door on the wall of the eye (sclera).
● Applying an anti-scarring medication (mitomycin-C) to prevent the trap
door from scarring.
● Creating a channel in the sclera (sclerostomy) and a hole in the iris
(iridectomy), to allow aqueous to drain out from the eye.
● Tightening the trap door with stitches. This limits the flow of aqueous out
of the eye, and prevents low eye pressure due to uncontrolled drainage
of aqueous. These stitches can be removed or cut with laser later on
to increase aqueous drainage.
● Covering the trap door with the conjunctiva (transparent skin overlying the
sclera). This forms a pocket of fluid called a ‘bleb’.
Aqueous will drain from the eyeball into the bleb (via the sclerostomy and trap door) and become absorbed by the surrounding blood vessels. This decreases the eye pressure.
See Related:
XEN gel stent implantation for glaucoma
Drainage tube shunt surgery for glaucoma
What are the potential risks?
Trabeculectomy has a success rate of around 70-80%. Most complications can be treated, although sight-threatening complications may occur rarely (less than 1 in every 1000). These can sometimes occur even if the operation has been carried out perfectly.
If you have severe glaucoma, there is a risk of completely losing all vision due to the stress of the procedure (snuff-out).
Risks during surgery:
● Bleeding into the eye. If severe the operation may be discontinued, and
will need to be completed on another day.
● Damage to other parts of the eye. This will prolong the surgery and your
eye may take a few months to recover instead of a few weeks.
Risks after surgery, where treatment does not involve another procedure:
● Bruising of the eye or eyelids. This is quite common.
● Allergy to the post-surgery eye drops, causing redness and irritation of
the eye and eyelid.
● High pressure in the eye. The pressure can be reduced by releasing
aqueous from the eye, massaging the eye, or by removing or cutting the
trap door stitches. However, if the pressure remains persistently high, you
may require pressure-lowering drops or tablets.
● Low pressure in the eye (hypotony). This usually settles over the course
of several weeks to months. Occasionally, it can be severe and cause
reduced vision in the long term.
Risks after surgery, where treatment requires another surgical procedure:
● Bleb leak. This may cause the eye pressure to become low and increases
the risk of infection. The leak can sometimes heal with the aid of contact
lenses, but usually requires treatment with a bleb revision procedure.
● Bleb failure. Scarring of the trap door and bleb prevents aqueous from
draining out of the eye. During your postoperative visits, you may receive
multiple injections of anti-scarring medication (5-fluorouracil) around the
trap door and bleb to try to prevent the scar tissue from forming.
Sometimes the scar tissue needs to be cut with a blade or needle to free
up the trap door and bleb (bleb needling procedure).
● Infection inside the eye (endophthalmitis). This is the most serious
complication and may cause permanent sight loss despite treatment with
antibiotics and surgery.
● Cloudiness of the lens in the eye (cataract). This can be treated with
cataract surgery.
● Droopiness of the eyelid (ptosis). This is usually mild. However if this
causes problems, the eyelid can be lifted by tightening the eyelid muscle
(ptosis surgery).
See Related: Risks and complications of glaucoma surgery
What should I expect?
Trabeculectomy is a hospital-based day case procedure performed under local anesthetic. The operation is usually performed one eye at a time.
Before surgery:
On the day of your procedure, please take all your usual medications unless otherwise advised. You will need to fast for at least 6 hours before your procedure. You will not be able to drive home on the day of the procedure, so you will need to arrange for someone to take you home. Please allow at least 3 to 4 hours in the hospital.
Before the trabeculectomy procedure, you will receive the following:
● Eye drops to constrict the pupil. These can take up to 30 minutes to work.● Cannula inserted into a vein, usually at the back of your hand.
● Local anesthetic eye drops prior to the anesthetic injection.
● Local anesthetic injection into the eye socket to fully numb the eye.During surgery:
To reduce the risk of infection, povidone iodine antiseptic is used to clean your eye and eyelashes, a sterile drape will cover your face, and a sterile clip will keep your eyelids open.
You will be awake during surgery, but you should not feel any pain. If you feel discomfort or pain, additional local anesthetic can be given. It is normal to notice bright lights or colors, hear buzzing and beeping sounds, and feel cold water running down your cheek or ear.
You will need to lie relatively still for up to 90 minutes for the operation. At the end of surgery, you may feel a sting due to an injection.
After surgery:
After trabeculectomy, a pad and shield will be placed over your eye. The pad and shield can be removed the next day, and you can start your postoperative eye drops. These comprise:
● Steroid anti-inflammatory eye drops (Prednisolone or Dexamethasone)
2-hourly for 4 to 6 weeks. These drops will be decreased gradually over
several months.
● Antibiotic eye drops (Chloramphenicol) 4 times daily for 1 week.
● Steroid eye ointment (Hydrocortisone) at night for 1 month.
You will need to stop your glaucoma eye drops (if any) to the operated eye. However, please continue your usual eye drops to the non-operated eye.
Over the next few weeks, you will experience blurriness, discomfort, sensitivity to light, and blood around the eye. These will gradually improve over several weeks with the eye drops. Please avoid strenuous activity during this period.
You will be reviewed the next day, and then weekly for a few weeks after trabeculectomy. During these visits, you may receive injection of an anti-scarring medication (5-fluorouracil) around the bleb. The visits (and injections) will become less frequent as the eye settles.
Please contact the clinic immediately if you experience pain or a sharp drop in vision.
See Related:


