
What is viral conjunctivitis?
Viral conjunctivitis (also known as pink eye) is the inflammation of the conjunctiva when it is caused by infection with a virus.
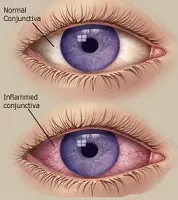
The conjunctiva is the thin, transparent layer that lines the front of the sclera (white part of the eye) and the inner surface of the eyelids. The conjunctiva It is usually colorless (apart from some blood vessels), but becomes pink or red when there is inflammation (see right).
The commonest viruses causing conjunctivitis are:
– Adenovirus(also causes the common cold)
– Molluscum contagiosum (also causes a typical skin rash)
– Herpes simplex virus
– Herpes zoster
Most of the time, viral infections of the conjunctiva are CONTAGIOUS. These viruses spread through air droplets and direct contact. Contaminated hands, towels, door handles, swimming pool water and children are particular culprits. The conjunctivitis remains contagious for as long as the eyes are inflamed.
What happens when I get viral conjunctivitis?

Conjunctivitis is the most common complaint. The conjunctiva becomes red and irritated (see left). There is usually yellow-ish discharge from the eye, and the eyelids are difficult to open in the morning (this is also known as morning stickiness).
You may also notice increased sensitivity to light and increased eyelid puffiness. Often, the conjunctivitis is preceded by flu or cold symptoms. The bad news is that the infection will almost always spread to the other eye within a few days.
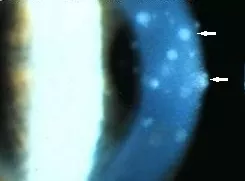
Keratitis develops when the cornea (clear window at the front of the eye) also becomes involved. This shows up as superficial white spots on the cornea (see right; white arrows). Keratitis occurs when the infection is more severe, and may cause scarring of the cornea that is significant enough to impair vision.

Molluscum contagiosum is a common skin infection causing small, raised nodules on the skin. Molluscum of the eyelid (see left; red arrow) can cause chronic conjunctivitis.
How is viral conjunctivitis diagnosed?
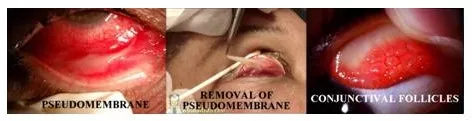
The diagnosis is usually obvious clinically. Apart from conjunctivitis, keratitis and skin molluscum, your ophthalmologist will also look for other clinical features including enlarged lymph nodes, subconjunctival hemorrhage, pseudomembranes, and conjunctival follicles (see below). However, if the diagnosis is in doubt, a swab from the conjunctiva can be taken and sent for analysis with polymerase chain reaction (PCR). PCR will detect the DNA of the virus that is causing the infection, thus confirming diagnosis.
How is viral conjunctivitis treated?
Conjunctivitis is a self-limiting disease, and generally resolves without treatment within two to six weeks. Often, the conjunctivitis worsens initially in the first week before improving. Most of the time, recovery is complete without any permanent or serious visual problems.
Treatment is usually for symptomatic relief, and may include the following:
Lubricating eye drops are useful to soothe the eyes when they are feeling gritty or uncomfortable. Any artificial tear eye drops, gels or ointment used for dry eye treatment will do.
Antibiotic eye drops / ointment are generally not recommended for viral infections. However, a short course of chloramphenicol, ofloxacin or fucidic acid is sometimes indicated if there is suspected bacterial infection on top of the viral infection.
Steroid eye drops, such as prednisolone, dexamethasone, or fluorometholone are indicated when the conjunctivitis is severe, especially when there is also keratitis. Steroids have no anti-viral activity; what they do is to help settle down the inflammation and reduce the risk of conjunctival and corneal scarring. The steroid eye drops need to be weaned off once the inflammation starts to clear. Ocular use of steroid, especially if long-term, can be associated with glaucoma and cataract.
Hygiene is absolutely crucial because of how contagious the disease is. Always wash your hands thoroughly, and avoid touching or rubbing your eyes, sharing towels and shaking hands. You may wish to consider changing your pillow case everyday to avoid reinfecting your eyes. If you wear contact lenses, stop wearing them until the conjunctivitis has completely resolved. You may have to stay home for at least a week (or even longer) until you are no longer contagious to avoid infecting your work or school mates.


